Commonly tested dermatology concepts on the USMLE: An updated guide




Table of contents
- Stay ahead of USMLE dermatology trends
- Master integrated clinical reasoning: Excelling on contemporary USMLE dermatology questions
- Maximize your USMLE score by mastering current high-yield and emerging dermatology topics
- Why scenario-based reasoning is essential for USMLE dermatology success
- Mastering interdisciplinary integration for complex USMLE dermatology cases
- Strategic tracking of USMLE dermatology exam trends for optimal preparation
This article is part 5 of 6 in our USMLE dermatology series, where we provide you with all the information you need to study for and ace dermatology-related questions and vignettes on your medical residency exams. In part 5, we outline strategies for integrating clinical reasoning and comprehension with real-world scenarios, ensuring the material you're covering closely reflects what's on the actual exam.

Stay ahead of USMLE dermatology trends
Master integrated clinical reasoning: Excelling on contemporary USMLE dermatology questions
As a USMLE candidate aiming for top performance, it's essential to understand that dermatology questions now test your clinical integration skills - not just your memory. The exams expect you to synthesize clinical presentations with histopathology, epidemiology, and pathophysiology. For example, you may encounter a patient vignette with a rapidly growing, irregularly pigmented lesion, accompanied by a photomicrograph (showing atypical melanocytes at the dermal-epidermal junction) and a history of extensive sun exposure. You'll need to connect history, labs, and histology to diagnose and manage conditions like malignant melanoma or chronic actinic dermatitis.
According to the USMLE Step 1 Clinical Vignette Analysis by Ace Med Boards, you'll be expected to:
- Precisely correlate histopathologic features - for instance, identifying spongiosis in eczema, parakeratosis in psoriasis, or atypical melanocytes in melanoma
- Apply epidemiological context - such as recognizing heightened melanoma risk in individuals with Fitzpatrick skin types I-II and significant UV exposure
- Integrate physical exam findings and diagnostic results - like associating a positive Nikolsky sign and biopsy-confirmed intraepidermal clefting with pemphigus vulgaris (AMBOSS Principles of Dermatology Overview)
- Interpret a variety of data types, including adverse event reports and clinical trial abstracts (USMLE Step 3 Formats and Sample Questions)
You'll often face cases where superficially similar findings, like erythematous, scaly plaques, require you to analyze underlying pathophysiology and context to distinguish between entities such as psoriasis (silvery scale, Auspitz sign) and lichen planus (Wickham striae, mucosal involvement). Excelling requires you to consistently connect clinical findings to their molecular or immunologic mechanisms and make evidence-based management decisions.
The Comprehensive USMLE Content Outline emphasizes the trend toward integrated, interdisciplinary questions. High-achieving examinees set themselves apart by analyzing complex information and applying advanced reasoning rather than relying solely on memorization.
Maximize your USMLE score by mastering current high-yield and emerging dermatology topics
To score highly, focus your preparation on both classic and emerging dermatology topics that frequently appear on the USMLE:
1. Drug-induced skin reactions: Understanding hypersensitivity mechanisms
- Type IV (delayed, T-cell mediated) reactions: Expect vignettes involving allergic contact dermatitis from nickel, presenting as pruritic, linear vesicles 48-72 hours post-exposure. Be prepared to explain the role of T-cell activation and cytokine release. (USMLE Drug Reactions Video Walkthrough)
- Serum sickness (Type III hypersensitivity): Look for polyarthralgia, urticarial rash, and hypocomplementemia 10-14 days after beta-lactam use.
2. Genetic dermatologic syndromes: Current exam priorities
- Xeroderma pigmentosum: Know its autosomal recessive inheritance, nucleotide excision repair defect, and high risk for early-onset skin cancers.
- Dermatitis herpetiformis: Be able to identify grouped vesicles on extensor surfaces, HLA-DQ2/DQ8 association, and the link to celiac disease via anti-tissue transglutaminase antibodies. (Comprehensive Dermatitis Herpetiformis Review Video)
3. Rare but frequently tested conditions: USMLE overrepresentation
- Staphylococcal scalded skin syndrome (SSSS): Common in pediatric vignettes, presenting with acute erythema, desquamation, and a positive Nikolsky sign due to Staphylococcus aureus exfoliative toxin. This is a favorite for questions due to its clear features and emergent nature (Medbullets Step 2 Dermatology Dashboard; Expert Analysis of High-Yield Dermatology Concepts).
"These rare conditions are tested more often because they have clear diagnostic criteria and represent clinical emergencies that demand immediate recognition."
Strategic insight: USMLE questions consistently highlight topics with systemic implications, urgent clinical significance, and distinct diagnostic features. Mastering these will enable you to rapidly recognize and manage them on exam day.

Why scenario-based reasoning is essential for USMLE dermatology success
As a USMLE examinee, you'll encounter scenario-based questions that require you to go beyond visual identification. To excel, you need to:
- Build differential diagnoses using history and risk factors (e.g., distinguishing Stevens-Johnson syndrome from erythema multiforme based on drug exposure or HSV infection)
- Justify your management and rule out mimics
- Tailor treatment to individual variables, such as immunosuppression or pregnancy status
Your USMLE success depends on your ability to:
- Prioritize differential diagnoses with a rich clinical context
- Adapt treatment plans to patient-specific risks
- Identify when referrals or urgent action are warranted
You should prioritize scenario-driven practice that challenges your critical thinking and clinical justification skills.
Mastering interdisciplinary integration for complex USMLE dermatology cases
USMLE cases often require integrating dermatologic findings with laboratory and systemic features, and knowing when to consult specialists. For maximum exam success, you should focus on:
- Correlating clinical and lab data: For example, diagnosing pemphigus vulgaris by integrating flaccid intraepidermal blisters, anti-desmoglein IgG, and net-like immunofluorescence
- Navigating specialty collaboration: Cases like dermatomyositis require you to recognize Gottron's papules, proximal muscle weakness, and the need for cancer screening/rheumatology referral
- Connecting systemic disease: Bullous pemphigoid questions assess your ability to link tense subepidermal blisters, linear IgG/C3 at the basement membrane, and neurologic disease associations
- Employing cross-disciplinary reasoning: For dermatitis herpetiformis, you must connect neutrophilic microabscesses on biopsy with celiac disease
- Evaluating prognosis: In melanoma, proficiency in Breslow thickness, ulceration, and mitotic rate informs prognosis and surgical planning
Top-scoring examinees consistently integrate diverse data, formulate management that addresses both immediate and long-term needs, and recognize when escalation is indicated.
Strategic tracking of USMLE dermatology exam trends for optimal preparation
For those targeting high Step 2 CK scores and competitive residencies, staying current with USMLE dermatology trends is non-negotiable. With Step 1 now pass/fail, Step 2 CK and research productivity weigh more heavily in residency selection. Notably, from 2020 to 2024, unmatched applicants with Step 2 CK scores above 250 doubled, underscoring the competitive landscape (Dermatology Residency Match Data and Trends, 2020-2024).
Implications for your study plan:
- Disregard outdated topic lists and score benchmarks. Prioritize up-to-date exam trends and program expectations.
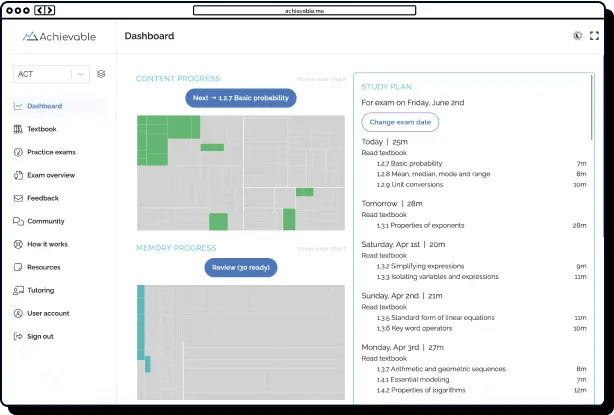
- Regularly consult USMLE bulletins and analytics from trusted prep platforms (e.g., MedBullets, USMLEStrike) for real-time updates (Atlas Blog: Essential USMLE Skin & Tissue Strategies).
- Focus on mastering:
- Complex clinical patterns
- Diagnostic criteria and first-line management
- Disease associations involving dermatology, immunology, and pharmacology
A recent survey found that most dermatology program directors prioritize clinical reasoning and systems-based judgment over rote memorization (Dermatology Application Trends After Step 1 Pass/Fail).
Action steps:
- Set regular (e.g., quarterly) check-ins to review NBME and prep platform analytics.
- Update your study schedule to cover topics gaining prominence, such as autoimmune pathways in vitiligo or novel psoriasis treatments.
- Top USMLE scorers dedicate about a fifth of their study time to analyzing trends and incorporating new content.
By systematically tracking exam trends and refining your preparation, you'll ensure your dermatology knowledge is sharply focused - equipping you to excel on both current and evolving USMLE content.
Our closing entry in our series is called "Avoid classic pitfalls with structured approaches and memory tools." Read on for expert study advice so you can excel at active recall and build long-term retention of complex medical topics.